Understanding Osteomyelitis and Its Risks
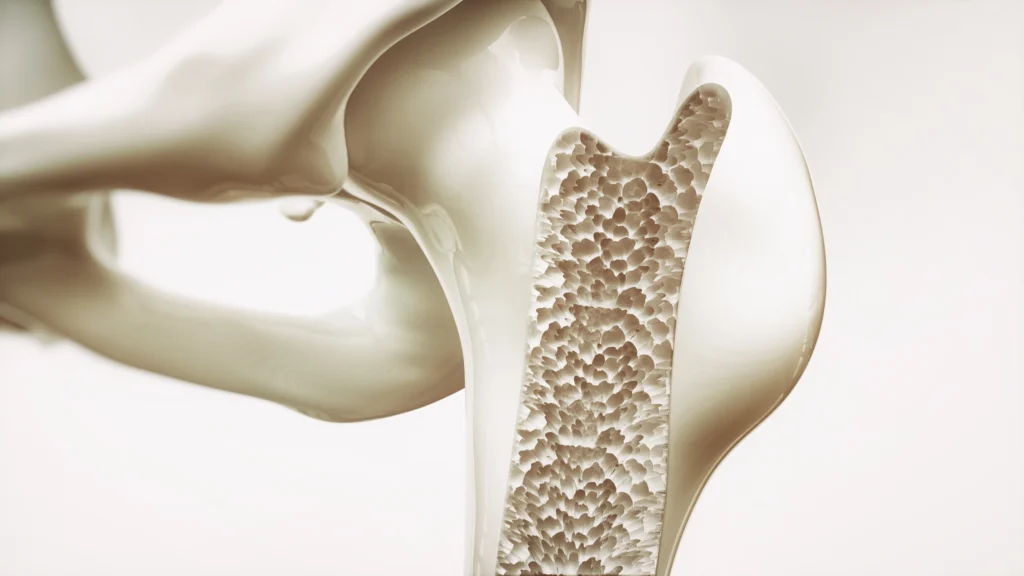
Osteomyelitis is a severe bone infection that requires prompt diagnosis and targeted treatment to prevent long-term complications, including the risk of amputation. This condition commonly affects individuals with diabetes, particularly those with diabetic foot ulcers. When circulation is compromised, the body’s ability to deliver oxygen and fight infection is significantly reduced, increasing the likelihood of bone damage and necrosis.
Among individuals with diabetic foot ulcers, more than 20% will develop osteomyelitis. Diabetic neuropathy further complicates early detection, as patients may not experience pain or notice infection-related symptoms. If left untreated, this condition can become chronic and difficult to manage.
However, osteomyelitis is not exclusive to diabetic patients. It can arise after trauma, puncture wounds, or as a complication of joint replacement surgery. Individuals with weakened immune systems, such as those undergoing hemodialysis, are also at increased risk. The growing prevalence of antibiotic resistance makes early detection and intervention even more critical.

Recognizing Symptoms and the Importance of Early Diagnosis
Osteomyelitis symptoms may include:
• Swelling and redness around the affected area
• Burning sensations or pus drainage from a wound
• Fatigue and fever
• Persistent pain or tenderness
For individuals with diabetes, any of these symptoms should prompt immediate medical evaluation to prevent further complications. Delayed treatment increases the risk of chronic infection and amputation.
Diagnosis typically involves imaging studies such as MRI scans, bone cultures, biopsies, or bone scans. Blood tests can also provide insight by detecting elevated white blood cell counts, indicating an active infection. Rapid identification leads to better treatment outcomes and improved healing rates.
Specialized Osteomyelitis Treatment Options
Traditional Approaches
Early-stage osteomyelitis is often treated with a combination of aggressive antibiotic therapy and surgical debridement to remove infected tissue. However, in cases where the infection is deep-seated or resistant to conventional treatments, additional interventions may be necessary.
The Role of Hyperbaric Oxygen Therapy (HBOT) in Osteomyelitis Treatment
Hyperbaric oxygen therapy (HBOT) is an advanced treatment option for chronic osteomyelitis, particularly when standard wound care and antibiotics are insufficient. During HBOT, patients breathe 100% oxygen in a pressurized hyperbaric chamber, which significantly enhances the body’s healing processes.

The benefits of HBOT for osteomyelitis include:
• Increased oxygen supply to infected bone and surrounding tissue
• Enhanced white blood cell activity to fight infection
• Reduction in swelling and inflammation
• Stimulation of new blood vessel growth, promoting faster healing
Incorporating HBOT into a comprehensive wound care plan can improve outcomes, reduce the risk of amputation, and support overall tissue regeneration.
Preventative Measures for High-Risk Patients
For individuals with diabetes or other risk factors, proactive wound care is essential. Daily foot examinations can help detect ulcers or early signs of infection before they progress. Patients with non-healing wounds lasting more than 30 days should seek specialized care from a wound care expert.
A comprehensive treatment plan may include:
• Proper wound debridement and infection control
• Offloading pressure from affected areas
• Nutritional support for enhanced healing
• Vascular health assessment and management
At Encompass Healthcare, we specialize in advanced wound care solutions, including hyperbaric oxygen therapy, to help patients recover from osteomyelitis and other complex infections.
Sources:



